Abstract
The objective of the study was to develop and validate a prediction model that identifies COVID-19 patients at risk of requiring oxygen support based on five parameters: C-reactive protein (CRP), hypertension, age, and neutrophil and lymphocyte counts (CHANeL). This retrospective cohort study included 221 consecutive COVID-19 patients and the patients were randomly assigned randomly to a training set and a test set in a ratio of 1:1. Logistic regression, logistic LASSO regression, Random Forest, Support Vector Machine, and XGBoost analyses were performed based on age, hypertension status, serial CRP, and neutrophil and lymphocyte counts during the first 3 days of hospitalization. The ability of the model to predict oxygen requirement during hospitalization was tested. During hospitalization, 45 (41.8%) patients in the training set (n = 110) and 41 (36.9%) in the test set (n = 111) required supplementary oxygen support. The logistic LASSO regression model exhibited the highest AUC for the test set, with a sensitivity of 0.927 and a specificity of 0.814. An online risk calculator for oxygen requirement using CHANeL predictors was developed. “CHANeL” prediction models based on serial CRP, neutrophil, and lymphocyte counts during the first 3 days of hospitalization, along with age and hypertension status, provide a reliable estimate of the risk of supplement oxygen requirement among patients hospitalized with COVID-19.
Introduction
Since the first case in Wuhan, China, in December 2019, the novel coronavirus disease 2019 (COVID-19) has spread rapidly world-wide. The clinical course and outcome of COVID-19 varies markedly from asymptomatic and mild, to critical and lethal. While young people without underlying comorbidities tend to have asymptomatic or mild disease, elderly patients and those with comorbidities (such as cardiovascular disease, diabetes mellitus, hypertension, chronic lung disease, cancer, and chronic kidney disease) are at an increased risk of death from respiratory failure and sepsis1,2,3,4.
In the absence of effective and/or preventive treatments, the outcome for critically ill COVID-19 patients depends on the availability of supportive intensive medical care5.The rapid spread of COVID-19 as a global pandemic has brought extraordinary challenges to the healthcare system. When the healthcare system is overwhelmed by a massive influx of patients, mortality increases6.In the face of limited resources, it is critical to reliably identify COVID-19 patients who require close monitoring and intensive care, including supplementary oxygen and/or mechanical ventilation, while those patients with a good prognosis can be monitored at home or managed at a living and treatment center7.A prediction model that can identify patients at high risk of respiratory failure at an early stage will help optimal allocation of limited resources.
During the early stage of COVID-19 infection, immunologic responses differ between survivors and non-survivors2.Since clinical and laboratory parameters (especially inflammatory markers) are subject to dynamic change, trends (i.e., time-series measurements) might better capture onset of a potentially lethal hyper-inflammatory immune response, which is associated with a severe clinical course and a poor outcome8.
Here, we aimed to construct a prediction model that identifies COVID-19 patients at high risk of developing respiratory failure. Based on our previous findings, we a priori selected five parameters: CRP, hypertension status, age, and neutrophil and lymphocyte counts (CHANeL). We hypothesized that the pattern of CRP, and neutrophil and lymphocyte counts during the first 3 days of hospitalization are predictive of the type (e.g., hyper-inflammatory) of inflammatory response likely to occur during the course of infection. We constructed several prediction models including a logistic regression, logistic LASSO regression, a Random Forrest model, a Support Vector Machine, and XGBoost. We found that the logistic LASSO regression model showed high sensitivity and specificity for identifying patients with COVID-19 who are at high risk of respiratory failure during hospitalization.
Results
Baseline characteristics
Between January 24, 2020 and July 10, 2020, 280 consecutive patients with COVID-19 were enrolled. After excluding patients with an unclear diagnosis (n = 3) and missing data (n = 56), 221 patients were assigned randomly to a training set (n = 110) or a test set (n = 111) (Fig.1).The mean age of the patients in the training and test sets was 56.0 and 55.0 years, respectively, and 58.2% and 65.8%, respectively, were male. The clinical characteristics of the patients in the training and test sets at the time of admission are shown in Table1.There was no difference in baseline pulse oximetric saturation/fraction of inspired oxygen (SpO2/FiO2) ratio and other clinical and laboratory features between the groups. The prevalence of hypertension, diabetes and chronic kidney disease were similar in the training set and the test set (Table1.) Forty-six patients (41.8%) in the training set and 41 (36.9%) in the test set required supplementary oxygen during hospitalization. The patients received supplementary oxygen therapy when clinically indicated (SpO2 < 92% or any shortness of breath on room air). The mode of oxygen administration was subject to change based on the patient’s condition as described in Supplementary TableS2.
Study design and patient flow.*National Medical Center (n = 128), Seoul National University Hospital (n = 46), Armed Forces Capital Hospital (n = 41), Myongji Hospital (n = 40), and Seoul National University Bundang Hospital (n = 25). ALC, absolute lymphocyte count; ANC, absolute neutrophil count; CRP, C-reactive protein.
Prediction models
我们开发了多元风险作表语用tion models to assess the primary outcome (i.e., requirement of supplementary oxygen during hospitalization) based on five variables. All five models showed a high AUC > 0.9 for the training set and test set. Among them, the logistic LASSO regression model showed the highest AUC for the test set (Fig.2A,B).
Receiver operating characteristic curve (ROC) and radar plot showing the performance of five different prediction models. (A) ROC curve for the training set. (B) ROC curve for the test set. (C) Radar plot for the training set. (D) Radar plot for the test set. AUC, area under the curve; NPV, negative predictive value; PPV, positive predictive value.
Sensitivity and specificity of the prediction models
The probability cut-off for each model was set at 0.3 to increase the sensitivity (at the cost of specificity). Sensitivity, specificity, predictive values, and accuracy of the predictor models for both the training and test set were high (Table2and Fig.2C,D). Among the test models, the logistic LASSO regression model showed the highest sensitivity (0.927) and specificity (0.814) for the test set. All models had a high negative predictive value (NPV). When the probability cut-off value was set to > 0.4, the specificity (for the training and test set) and accuracy (for the training set) improved, but the sensitivity decreased.
Estimated predictive value of the CHANeL parameters
The individual contribution of each of the five predictors was estimated (Supplementary TableS1).在物流LASSO regression model, the CRP value on Day 3 had the highest impact in all five models, whereas the CRP level on Days 1 and 2 played less of a role. In the Random Forest model, variables of the first 3 days were important.
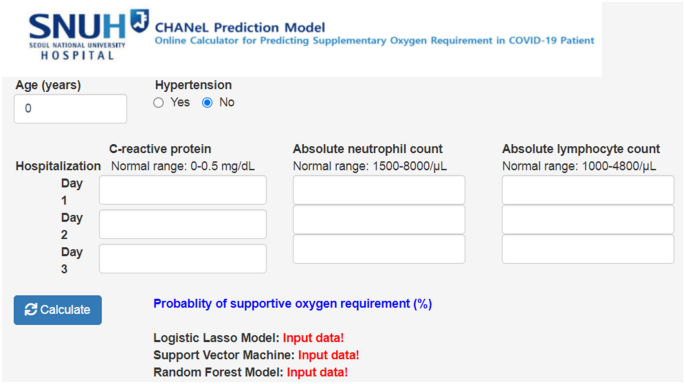
Construction of a calculator
An online calculator based on the logistic LASSO regression model and the Random Forest model using the CHANeL predictors was developed to calculate the risk score for a hospitalized patient with COVID-19 requiring supplementary oxygen during hospitalization (http://166.104.118.164:3838/chanel/) (Fig.3).
Discussion
To the best of our knowledge, this study was the first attempt to include pattern of the routine inflammatory markers during the early stage of disease in model to predict requirement for supplementary oxygen (i.e., respiratory failure) among hospitalized patients with COVID-19. All models based on CHANeL (age, hypertension, serial CRP, and neutrophil and lymphocyte counts during the first 3 days of hospitalization) showed high accuracy.
The unique strength of the CHANeL prediction models is the hypothesis-driven a priori selection of the five predictors. We showed previously that a hyper-inflammatory immune response, characterized by high CRP levels, high neutrophil counts, and low lymphocyte counts, was associated with a requirement for supplementary oxygen support and a worse outcome, whereas a normal inflammatory response, characterized by minimal elevation of CRP, a normal neutrophil count, and a normal lymphocyte count, was associated with an excellent outcome8.The inflammatory markers were similar on day of admission and started to differ between patients who required supplementary oxygen and those who did not in the first few days of illness. The difference become prominent in the second week of hospitalization. Thus, the dynamic changes (i.e., patterns) in common inflammatory markers (CRP, and neutrophil and lymphocyte counts) in early disease course were strongly associated with overall inflammatory response and clinical severity of COVID198.A retrospective study of 136 COVID-19 patients showed that initial clinical and laboratory characteristics at admission were not predictive of this deterioration, further supporting that parameters measured at a single time point might not be sensitive enough to identify patients at risk9.To increase the model accuracy, we included two known demographic risk factors (age and hypertension), which have been identified consistently as demographic characteristics associated with a worse outcome2,5.
Numerous laboratory parameters have been suggested as risk factors for a worse outcome of COVID-19 disease; these include increased neutrophil counts, decreased lymphocyte counts (and, thus, the neutrophil/lymphocyte ratio), elevated CRP levels, and elevated d-dimer levels2,4,10,11,12,13.Others identified serum hydrogen sulfide and soluble urokinase plasminogen activator receptor as potential predictors for severe pneumonia in COVID-1914,15.Furthermore, blood levels of interleukin (IL)-1, IL-6, IL-8, and tumor necrosis factor (TNF) are associated with severity and prognosis of COVID-1916.TNF和il - 6驱动肝c反应蛋白的合成,当reas IL-8 increases neutrophil recruitment. Therefore, the levels of these cytokines are reflected indirectly by CRP levels and neutrophil counts in the CHANeL model. Liang et al. developed a clinical risk score to predict the probability of developing a critical illness. The score system was based on ten variables measured at admission, all of which were selected from an initial 72 candidates17.Similarly, the other prediction models for severe COVID-19 such as CANPT score or CMR tool are based on scoring of numerous parameters at admission18,19.By contrast, the CHANeL model is based on the hypothesis that the inflammatory response ultimately determines the clinical course of COVID-19. Since clinical manifestations such as hemoptysis, dyspnea, chest X-ray abnormalities, and mental status change, and laboratory parameters are considered to be the result (not the cause) of a systemic inflammatory response to viral infection, they were not included. Despite, or because of, its simplicity, the performance of the CHANeL-based prediction models was high; all models had an AUC of > 0.9 (Fig.1).The five different models were indirectly compared with regards to sensitivity, specificity, positive predictive value, negative predictive value and accuracy, and the logistic LASSO model and the Random Forrest Model showed the best sensitivity and specificity (Table2, Fig.2C); therefore, they were used to develop a risk calculator for bedside use (Fig.3).Interestingly, in the logistic LASSO model, day 3 level of the CRP (among the first 3 days values) had the highest impact. However, in other models, the values on day 1–3 (the “trend” over the first 3 days) were important (Supplementary tableS1), emphasizing the different algorithms used in the 5 prediction models.
Identifying patients with a hyper-inflammatory immune response early during the disease course may enable timely treatment of those at risk of high mortality. This is of particular interest since progression to acute respiratory distress syndrome or sepsis often marks the “point of no return”, where most treatment options (including high dose glucocorticoids) become ineffective20.Therefore, targeted blockade of additional detrimental hyper-inflammatory responses using early glucocorticoid and/or a monoclonal antibody (neutralizing proinflammatory IL-6) therapy might prevent exacerbation21,22.This can, optimally, facilitate allocation of limited resources during a pandemic (and prevent the collapse of the healthcare system); patients at a low risk can be discharged from hospital safely after 3 days of observation to self-quarantine at home or in a living and treatment center7, whereas patients at a high risk should remain in hospital for close monitoring and intensive treatment. Further studies are needed to investigate whether implementing the CHANeL model will save more lives and/or shorten hospital stay.
This study has several limitations. First, this study included only hospitalized Korean patients. External validation of the CHANeL models in different ethnic groups is required. Second, the mortality in this cohort was 2.7% whereas the current mortality of COVID-19 is 1.6% in Korea23.As the patients in this cohort only included hospitalized patients, the mortality was expected to be significantly higher than that in the general population, indicating that the relatively mild COVID-19 cases were included (58.2% of patients in the training set and 63.1% in the test set did not require any oxygen supplementation). This is, in part, due to the low incidence of COVID-19 in Korea, allowing the many patients with mild COVID-19 being treated as inpatients. The higher proportion of the non-O2 requirement, however, help to build the model better. Third, information on arterial blood gas analysis or PaO2/FiO2(PF) ratio was not available in all patients. Instead, we utilized SpO2/FiO2ratio which correlates with PF ratio24.Last but not the least, the primary aim of the study was to identify high risk patients who require more intensive monitoring and treatment (i.e. oxygen requirement as a surrogate marker for more severe disease). Therefore, an ideal study population would be patients who are just diagnosed with COVID-19. Accordingly, the prediction models need to be validated in a prospective cohort of patients who are diagnosed with COVID-19.
In conclusion, CHANeL prediction models based on serial measurements of CRP, ANC, and ALC during first 3 days of hospitalization, along with age and hypertension, provide an accurate estimate of the risk of supplement oxygen requirement among hospitalized patients with COVID-19. Further studies are needed to examine whether implementing this model at bedside can improve outcomes and shorten hospital stays.
Methods
Patients and data collection
这包括COVID-19回顾性队列研究patients who were treated at five medical centers designated for treatment of COVID-19 by the South Korean government. A diagnosis of COVID-19 was confirmed by a positive SARS-CoV-2 real-time reverse transcriptase–polymerase chain reaction result from a respiratory sample; RT-PCR was performed at the participating institutions or at the Korea Centers for Disease Control and Prevention. The cohort included 280 consecutive patients with COVID-19, all of whom were admitted to one of the five hospitals from January 24, 2020 through July 10, 2020. After excluding patients with incomplete information about medications, the patients were assigned randomly to a training set and a test set in a ratio of 1:1. Of note, the patients included in this study were the same as the patients included in our prior study8.
Demographic and laboratory data were obtained from electronic medical records. The study was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. The study was approved by the institutional review board of each participating center (NMC, SNUBH, SNUH, Armed Forces Capital Hospital, Myongji hospital). The institutional review board of each participating center (NMC, SNUBH, SNUH, Armed Forces Capital Hospital, Myongji hospital) waived informed consent because the study involved a minimum risk to the patient and no identifiable information was used.
Outcome
The primary outcome was a requirement for supplementary oxygen during the hospitalization period. Supplementary oxygen requirement, ranging from nasal prongs to mechanical ventilation, is a marker of COVID-19 severity and an important indication for close monitoring and treatment. A previous study showed that all patients with COVID-19 who did not require supplementary oxygen had a mild disease course and a good prognosis8.
Selection of CHANeL predictors
Two demographic variables (age and history of hypertension) were selected a priori; both of these are known risk factors for severe COVID-19 disease25.In addition, three routine inflammatory markers (CRP, absolute neutrophil count (ANC), and absolute lymphocyte count (ALC)) during the first 3 days of hospitalization were selected. Predictor selection was based on the previous observation that longitudinal patterns of CRP, ANC, and ALC are highly associated with a particular type of inflammatory response and clinical outcome, including oxygen requirement and death8.
Missing values were imputed using linear interpolation between the non-missing values immediately before and after the missing time point, with a calculated variation that follows the shape of the population’s average trajectory26.Patients for whom missing data could not be imputed reliably were excluded.
Construction of prediction models
Logistic regression, logistic LASSO regression, Random Forest, Support Vector Machine, and XGBoost analysis were tested using the five CHANeL predictors. The ability of each model to predict supplementary oxygen requirement was assessed by calculating the area under the receiver-operator characteristic curve (AUC). A training set and a test set was used to test each model for sensitivity (proportion of oxygen requirement cases predicted correctly), specificity (proportion of no-oxygen requirement cases predicted correctly), and accuracy (proportion of cases predicted correctly).
Statistical analysis
Continuous variables and categorical variables were compared using t-tests or the Mann–Whitney U-test, or the Chi-squared test or Fisher’s exact test, as appropriate. Statistical analysis was performed using RStudio (version 1.2; Boston, MA, USA) and SPSS (IBM SPSS Statistics for Windows, Version 25.0). AP-value < 0.05 was considered statistically significant.
References
Chan, J. F.et al.A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster.Lancet395, 514–523.https://doi.org/10.1016/S0140-6736(20)30154-9(2020).
Zhou, F.et al.Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study.Lancethttps://doi.org/10.1016/S0140-6736(20)30566-3(2020).
Onder, G., Rezza, G. & Brusaferro, S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy.JAMAhttps://doi.org/10.1001/jama.2020.4683(2020).
Barison, A.et al.Cardiovascular disease and COVID-19: les liaisons dangereuses.Eur J Prev Cardiol27, 1017–1025.https://doi.org/10.1177/2047487320924501(2020).
Wu, Z. & McGoogan, J. M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention.JAMAhttps://doi.org/10.1001/jama.2020.2648(2019).
Rubino, S., Kelvin, N., Bermejo-Martin, J. F. & Kelvin, D. As COVID-19 cases, deaths and fatality rates surge in Italy, underlying causes require investigation.J Infect Dev Ctries14, 265–267.https://doi.org/10.3855/jidc.12734(2020).
Choe, P. G.et al.Selecting coronavirus disease 2019 patients with negligible risk of progression: Early experience from non-hospital isolation facility in Korea.Korean J. Intern. Med.35, 765–770.https://doi.org/10.3904/kjim.2020.159(2020).
李,E。E.et al.Pattern of inflammatory immune response determines the clinical course and outcome of COVID-19: Unbiased clustering analysis.Sci. Rep.11, 8080.https://doi.org/10.1038/s41598-021-87668-z(2021).
Suh, H. J.et al.Clinical characteristics of COVID-19: Clinical dynamics of mild severe acute respiratory syndrome coronavirus 2 infection detected by early active surveillance.J. Korean Med. Sci.35, e297 (2020).
Tan, L.et al.Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study.Signal Transduct Target Ther.5, 33.https://doi.org/10.1038/s41392-020-0148-4(2020).
Lippi, G. & Plebani, M. Laboratory abnormalities in patients with COVID-2019 infection.Clin. Chem. Lab. Med.https://doi.org/10.1515/cclm-2020-0198(2020).
Zhang, L.et al.D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19.J. Thromb. Haemost.https://doi.org/10.1111/jth.14859(2020).
Feng, X.et al.Immune-inflammatory parameters in COVID-19 cases: a systematic review and meta-analysis.Front. Med.7, 301.https://doi.org/10.3389/fmed.2020.00301(2020).
Rovina, N.et al.Soluble urokinase plasminogen activator receptor (suPAR) as an early predictor of severe respiratory failure in patients with COVID-19 pneumonia.Crit. Care (Lond. Engl.)24, 187.https://doi.org/10.1186/s13054-020-02897-4(2020).
Renieris, G.et al.Serum Hydrogen Sulfide and Outcome Association in pneumonia by the SARS-CoV-2 coronavirus.Shock (Augusta Ga.)54, 633–637.https://doi.org/10.1097/SHK.0000000000001562(2020).
Del Valle, D. M.et al.An inflammatory cytokine signature predicts COVID-19 severity and survival.Nat Med.26(10), 1636–1643,https://doi.org/10.1038/s41591-020-1051-9(2020).
Liang, W.et al.Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19.JAMA Intern Medhttps://doi.org/10.1001/jamainternmed.2020.2033(2020).
Chen, Y.et al.CANPT score: A tool to predict severe COVID-19 on admission.Front. Med.8, 68.https://doi.org/10.3389/fmed.2021.608107(2021).
Bertsimas, D.et al.新型冠状病毒肺炎mortality risk assessment: An international multi-center study.PLoS ONE15, e0243262–e0243262.https://doi.org/10.1371/journal.pone.0243262(2020).
Kim, H. I. & Park, S. Sepsis: Early recognition and optimized treatment.Tuberc Respir Dis (Seoul)82, 6–14.https://doi.org/10.4046/trd.2018.0041(2019).
Group, R. C.et al.Dexamethasone in hospitalized patients with Covid-19—Preliminary report.N Engl J Medhttps://doi.org/10.1056/NEJMoa2021436(2020).
Klopfenstein, T.et al.Impact of Tocilizumab on mortality and/or invasive mechanical ventilation requirement in a cohort of 206 COVID-19 patients.Int. J. Infect. Dis.https://doi.org/10.1016/j.ijid.2020.08.024(2020).
CSSEGISandData/COVID-19.https://github.com/CSSEGISandData/COVID-19.
Rice, T. W.et al.Comparison of the SpO2/FIO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or ARDS.Chest132, 410–417.https://doi.org/10.1378/chest.07-0617(2007).
Wu, C.et al.Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China.JAMA Intern. Med.180, 934–943.https://doi.org/10.1001/jamainternmed.2020.0994%JJAMAInternalMedicine(2020).
Genolini, C., Écochard, R. & Jacqmin-Gadda, H. Copy mean: A new method to impute intermittent missing values in longitudinal studies.Open J. Stat.3, 26–40.https://doi.org/10.4236/ojs.2013.34A004(2013).
Acknowledgements
None.
Funding
This work was supported by the New Faculty Startup Fund from Seoul National University.
Author information
Authors and Affiliations
Contributions
Conceptualization and design: J.K.P. and E.E.L. Data acquisition: K-H.S, BS.C., N.J.K., J.J., J-H.K., H.S.O., Y.M.K., and C.K.K. Data curation and formal analysis: E.E.L., K-H.S., W.H., and J.K.P. Statistical analysis: W.H. and E.E.L. Developing the prediction model and web tool: W.H and W.S. Writing the original draft: J.K.P. and E.E.L. Manuscript review and editing: K-H.S., BS.C., E.B.L., J.K.P., E.E.L. and N.J.K. All authors contributed to data interpretation and critical revision of the manuscript. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open AccessThis article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
李,E。E., Hwang, W., Song, KH.et al.Predication of oxygen requirement in COVID-19 patients using dynamic change of inflammatory markers: CRP, hypertension, age, neutrophil and lymphocyte (CHANeL).Sci Rep11, 13026 (2021). https://doi.org/10.1038/s41598-021-92418-2
Received:
Accepted:
Published:
DOI:https://doi.org/10.1038/s41598-021-92418-2
This article is cited by
Laboratory markers of severity across three COVID-19 outbreaks in Australia: has Omicron and vaccinations changed disease presentation?
Internal and Emergency Medicine(2023)
Predicting the necessity of oxygen therapy in the early stage of COVID-19 using machine learning
Medical & Biological Engineering & Computing(2022)
Comments
By submitting a comment you agree to abide by ourTermsandCommunity Guidelines.If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.